The purpose of this paper is to study and realise the patient is undergoing cardiopulmonary disease process, determination of respiratory care diagnoses, the formation of consequences with interventions, assessment of the outcomes based on the patient's situation with available subjective and objective data.
On January 31, 93 years old female admitted to the emergency room (ER) from nursing home facilities because of facial droop, left arm drift, stoke like symptoms, shortness of breath, and anxiety. The diagnosis revealed an acute hypoxic respiratory failure. The patient past cardiopulmonary disease history showed that chronic obstructive pulmonary disease (COPD), coronary artery disease (CAD), congestive heart failure (CHF), Atrial fibrillation (Afib), and breast cancer with Mets and recent diagnosis on Femera. Her past surgery included cardiac appendectomy in 2009, spine surgery in 2010, and ablation in 2014. Previously, she smoked one pack of cigarette per day but quit 30 years ago. According to family history, her father had diabetes; Mom had breast cancer, basal cell carcinoma (son), brain cancer (brother), and endometrial cancer (daughter and sister)
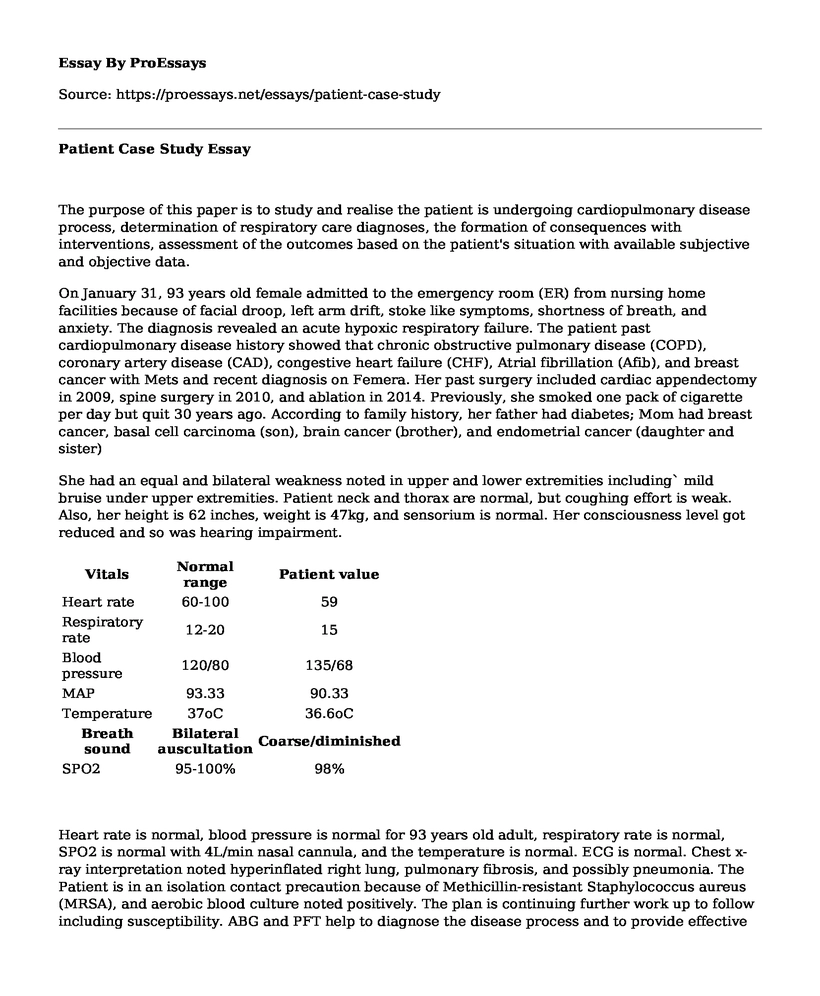
She had an equal and bilateral weakness noted in upper and lower extremities including` mild bruise under upper extremities. Patient neck and thorax are normal, but coughing effort is weak. Also, her height is 62 inches, weight is 47kg, and sensorium is normal. Her consciousness level got reduced and so was hearing impairment.
| Vitals | Normal range | Patient value |
| Heart rate | 60-100 | 59 |
| Respiratory rate | 12-20 | 15 |
| Blood pressure | 120/80 | 135/68 |
| MAP | 93.33 | 90.33 |
| Temperature | 37oC | 36.6oC |
| Breath sound | Bilateral auscultation | Coarse/diminished |
| SPO2 | 95-100% | 98% |
Heart rate is normal, blood pressure is normal for 93 years old adult, respiratory rate is normal, SPO2 is normal with 4L/min nasal cannula, and the temperature is normal. ECG is normal. Chest x-ray interpretation noted hyperinflated right lung, pulmonary fibrosis, and possibly pneumonia. The Patient is in an isolation contact precaution because of Methicillin-resistant Staphylococcus aureus (MRSA), and aerobic blood culture noted positively. The plan is continuing further work up to follow including susceptibility. ABG and PFT help to diagnose the disease process and to provide effective treatment.
| CBC | Normal range | Patient value |
| RBC | 4.0-*1o12/L | 4.03 * 10L(normal) |
| WBC | 4.5 *- 11.0 * 109 / L | 9.4 * 109 /L (normal) |
| HCT | 35-45% | 37.6% (normal) |
| Platelets | 150-450 *109 /L | 119*109 /L (low) |
| Na | 135-145 mEq/L | 137mEq/L (normal) |
| K | 3.5-5 mEq/L | 3.5mEq/L (normal) |
| CO2 | 22-29mEq/L | 28mEq/L (normal) |
| Cl | 98-106mmol/L | 99mmol/L (normal) |
| Blood gases (venous) | Normal range | Patient value |
| PH | 7.31-7.41 | 7.49 (H) |
| PaCO2 | 41-51 | 48.1(normal) |
| PaO2 | 30-40 | 23 (low) |
| HCO3 | 23-29 | 36(High ) |
| HB | 12.0-15.5 | 13.6 (normal) |
The patient code status is don not resuscitate (DNR). The intervention was based on the code status and more on control pain level, promote rest, avert respiratory failure, increase oxygenation, close monitor chronic obstructive pulmonary disease (COPD) and heart disease. The intervention also includes oxygen therapy (4L/min), and medication such as Albuterol-Ipratropium (DUO_NEB) 2.5mg/0.5mg /3mL nebuliser Q6H, fluticasone - salmeterol (Advair Diskus) 100mcg/50mcg one puff BID, bronchial hygiene (sodium chloride 3% nebuliser solution 4mL and TID and intrapulmonary percussion ventilation (IPV) TID). DUO-NEB helps for bronchodilation, Advair is used to control chronic obstructive pulmonary disease and prevent inflammation, and IPV and sodium chloride 3% solution help for mucus clearance. Later on, Advair Discus is changed into to Budesonide (PULMICORT) 0.5mg/2mL nebuliser 0.5mg BID because it wasn't effective 93 years old patient to use DPI.
Home medications include Albuterol 2.5mg / inhalation budesonide 0.5mg nebuliser, 2L oxygen therapy, aspirin (OTC) 1 or 2 QH. For cancer or blood disorder(8mg/1vial), sol-Motor gets used. Lipitor (10 mg per day) gets used for to reduce the risk of heart attack coronary heart disease and heparin (8o unit/kg IV bolus then continuous infusion 18unit/kg/h) gets used as an anticoagulant.
Overall, the patient was in the hospital for two weeks then discharged. Oxygenation was improved, shortness of breath was solved, vitals were in good condition. She was awake and alert, but hearing impairment was unsolved. Cautious development of intervention and help to get positive results and improved the situation. The constant assessment, preparation and evaluation of objectives and intervention allowed care to be fitted to the individual patient needs, supporting patient and family.
Cite this page
Patient Case Study . (2022, Mar 29). Retrieved from https://proessays.net/essays/patient-case-study
If you are the original author of this essay and no longer wish to have it published on the ProEssays website, please click below to request its removal:
- Medical Essay on Chest Pain
- Essay Sample on Short-Term and Long-Term Goals for Blue Cross Shield Massachusetts
- Public Health: From Ancient Greece to Today - Essay Sample
- Essay Example on Brain Drain: Challenges in Healthcare Delivery in Underdeveloped Nations
- Essay Example on Sustainable Practices: Hospitality Companies' Push for Positive Change
- Essay Example on Canada's Division 8 FDR: Regulating New Drugs for Safety & Quality
- NONPF Core Competencies - Report Example