Save this form on your computer as a Microsoft Word document. You can expand or shrink each area as you need to include the relevant data for your client.
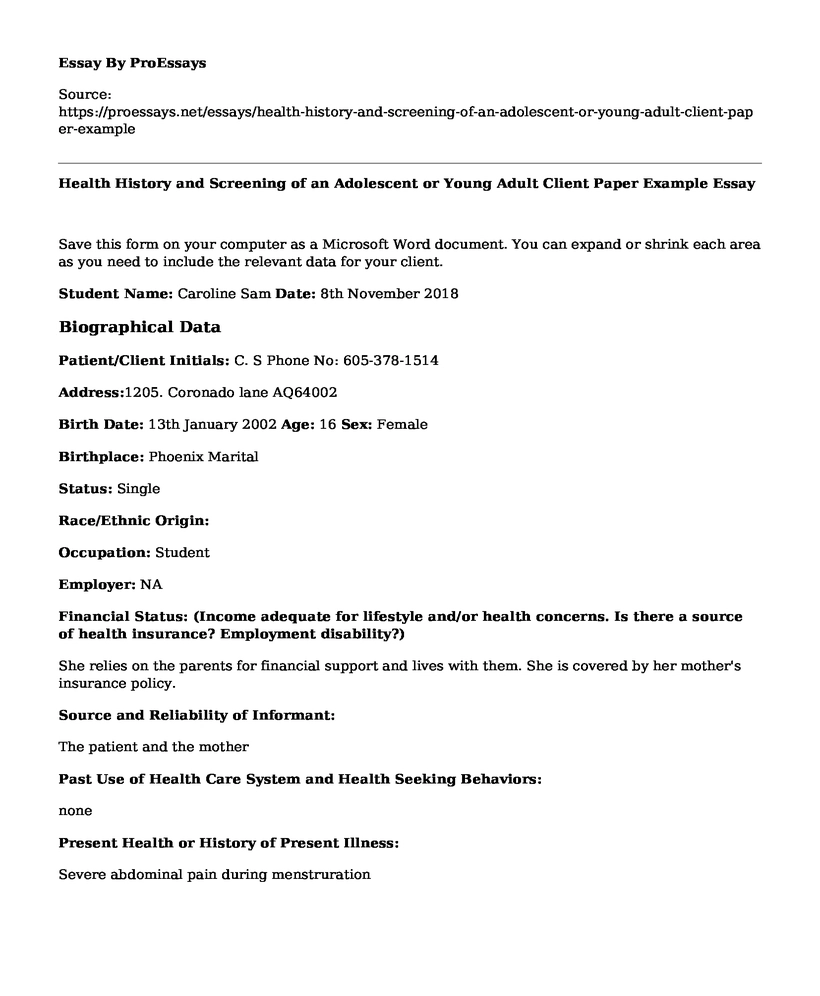
Student Name: Caroline Sam Date: 8th November 2018
Biographical Data
Patient/Client Initials: C. S Phone No: 605-378-1514
Address:1205. Coronado lane AQ64002
Birth Date: 13th January 2002 Age: 16 Sex: Female
Birthplace: Phoenix Marital
Status: Single
Race/Ethnic Origin:
Occupation: Student
Employer: NA
Financial Status: (Income adequate for lifestyle and/or health concerns. Is there a source of health insurance? Employment disability?)
She relies on the parents for financial support and lives with them. She is covered by her mother's insurance policy.
Source and Reliability of Informant:
The patient and the mother
Past Use of Health Care System and Health Seeking Behaviors:
none
Present Health or History of Present Illness:
Severe abdominal pain during menstruration
Past Health History
General Health: (Patient's own words)
- Has been having severe abdominal pains during her periods for the past three months.
- Has backaches too.
- Has diahorrehea or constipation too during her menses.
Allergies: (include food and medication allergies)
none
Reaction:
none
Current Medications:
Painkillers for the abdominal pains
Last Exam Date:
12th August 2018
Immunizations:
Yellow fever
Childhood Illnesses:
Bronchittis
Serious or Chronic Illnesses:
None
Past Health Screening (see "Well Young Adult Behavior Health Assessment History Screening" below)
Yearly pap smear and breast examination
Past Accidents or Injuries:
none
Past Hospitalizations:
Inpatient hospitalization for the treatment of bronchitis
Past Operations:
None
Family History
(Specify which family member is affected.)
Alcoholism (ETOH use/abuse):
Father
Allergies:
none
Arthritis:
Father
Asthma:
None
Blood Disorders:
None
Breast Cancer:
none
Cancer (Other):
none
Cerebral Vascular Accident (Stroke):
Father
Diabetes:
Mother
Heart Disease:
None
High Blood Pressure:
Grandmother
Immunological Disorders:
none
Kidney Disease:
Grandfather
Mental Illness:
none
Neurological Disorder:
none
Obesity:
None
Seizure Disorder:
none
Tuberculosis:
None
Obstetric History (if applicable)
Gravida: NA Term:NA Preterm:NA Miscarriage/Abortions:NA
Course of Pregnancy (length of pregnancy, delivery date, method of delivery, length of labor, complications, baby's weight, baby's condition):
NA
Well Young Adult Behavioral Health History Screening
Socio-Demographic Content and Questions:
What organizations or activities (community, school, church, lodge, social, professional, academic, sports) are you involved in?
- Sports and Church
How would you describe your community?
- Friendly
Hobbies, skills, interests, recreational activities?
- Good at badminton
- Sings in the church choir
Military service: Yes_______ No___X____
If yes, overseas assignment? Yes________ No__X_______
Close friends or family members who have died within past 2 years? Grandfather
Number of relatives or close friends in this area? five
Marital status: Single___X___ Married________Divorced_________Separated_________ In serious relationship________ Length of time_________
Environmental Content and Questions:
- Do you live alone?
Yes________ No _____X___
- When did you last move? Describe your living situation?
Living with the parents
- Number of years of education completed?
thirteen
- Occupation?
Student
- If employed, how long? Are you satisfied with this work situation? Do you consider your work dangerous or risky? Is your work stressful? Over the past 2 years have you felt depressed or hopeless?
no
Biophysical Content and Questions
- Have you smoked cigarettes? Yes_______ No_____X___
- How much?
- Less than pack per day_____ About 1 pack per day?______ More than 1 and packs per day______
- Are you smoking now? Yes_______ No____X____ Length of time smoking? ______________
- Have you ever smoked illicit drugs? Yes__________ No____X_____
- If yes, for how long? ___________ Do you smoke these now? Yes__________ No ___X_______
- Do you ingest illicit drugs of any kind? Yes_________ No____X______
- If so, what drugs do you use and what is the route of ingestion?_________
- How long have you used these drugs _________________
Review of Systems
(Include both past and current health problems. Comment on all present issues.)
General Health State (present weight - gain or loss, reason for gain or loss, amount of time for gain or loss; fatigue, malaise, weakness, sweats, night sweats, chills ):
- Present weight is at 50kgs
- Patient has lost 3kgs since the last check up
- Loss of appetite
Skin (history of skin disease, pigment or color change, change in mole, excessive dryness or moisture, pruritis, excessive bruising, rash or lesion):
none
Health Promotion (Sun exposure? Skin care products?):
Patient uses sunscreen
Hair (recent loss or change in texture):
NA
Health Promotion (method of self-care, products used for care):
NA
Nails (change in color, shape, brittleness):
NA
Health Promotion (method of self-care, products used for care):
NA
Head (unusual headaches, frequency of headaches, head injury, dizziness, syncope or vertigo):
none
Eyes (difficulty or change in vision, decreased acuity, blurring, blind spots, eye pain, diplopia, redness or swelling, watering or discharge, glaucoma or cataracts):
no
Health Promotion (wears glasses or contacts and reason, last vision check, last glaucoma check, sun protection):
no
Ears (earaches, infections, discharge and its characteristics, tinnitus or vertigo):
no
Health Promotion (hearing loss, hearing aid use, environmental noise exposure, methods for cleaning ears):
no
Nose and Sinuses (discharge and its characteristics, frequent or severe colds, sinus pain, nasal obstruction, nosebleeds, seasonal allergies, change in sense of smell):
no
Health Promotion (methods for cleaning nose)
hankerchief
Mouth and Throat (mouth pain, sore throat, bleeding gums, toothache, lesions in mouth, tongue, or throat, dysphagia, hoarseness, tonsillectomy, alteration in taste):
none
Health Promotion (Daily dental care - brushing, flossing. Use of prosthetics - bridges, dentures. Last dental exam/check-up.):
daily dental care and flossing
A month ago
Neck (pain, limitation of motion, lumps or swelling, enlarged or tender lymph nodes, goiter):
None
Neurologic System (history of seizure disorder, syncopal episodes, CVA, motor function or coordination disorders/abnormalities, paresthesia, mood change, depression, memory disorder, history of mental health disorders):
none
Health Promotion (activities to stimulate thinking, exam related to mood changes/depression):
meditation
Endocrine System (history of diabetes or insulin resistance, history of thyroid disease, intolerance to heat or cold):
None
Health Promotion (last blood glucose test and result, diet):
- Today
- 140mg/Dl (7.8 mmol/L)
Breast and Axilla (pain, lump, tenderness, swelling, rash, nipple discharge, any breast surgery):
NO
Health Promotion (performs breast self-exam - both male and female, last mammogram and results, use of self-care products):
Yearly breast examination
Respiratory System (History of lung disease, smoking, chest pain with breathing, wheezing, shortness of breath, cough - productive or nonproductive. Sputum - color and amount. Hemoptysis, toxin or pollution exposure.):
none
Health Promotion (last chest x-ray, smoking cessation):
none
Cardiac System (history of cardiac disease, MI, atherosclerosis, arteriosclerosis, chest pain, angina):
none
Health Promotion (last cardiac exam):
None
Peripheral Vascular System (coldness, numbness, tingling, swelling of legs/ankles, discoloration of hands/feet, varicose veins, intermittent claudication, thrombophlebitis or ulcers):
none
Health Promotion (avoid crossing legs, avoid sitting/standing for long lengths of time, promote wearing of support hose):
none
Hematologic System (bleeding tendency of skin or mucous membranes, excessive bruising, swelling of lymph nodes, blood transfusion and any reactions, exposure to toxic agents or radiation):
none
Health Promotion (use of standard precautions when exposed to blood/body fluids):
none
Gastrointestinal System (appetite, food intolerance, dysphagia, heartburn, indigestion, pain [with eating or other], pyrosis, nausea, vomiting, history of abdominal disease, gastric ulcers, flatulence, bowel movement frequency, change in stool [color, consistency], diarrhea, constipation, hemorrhoids, rectal bleeding):
- Low appetite
- Abdominal pain
Health Promotion (nutrition - quality/quantity of diet; use of antacids/laxatives):
laxatives
Musculoskeletal System (history of arthritis, joint pain, stiffness, swelling, deformity, limitation of motion, pain, cramps or weakness):
none
Health Promotion (mobility aids used, exercises, walking, effect of limited range of motion):
none
Urinary System (recent change, frequency, urgency, nocturia, dysuria, polyuria, oliguria, hesitancy or straining, urine color, narrowed stream, incontinence; history of urinary disease; pain in flank, groin, suprapubic region or low back):
none
Health Promotion (methods used to prevent urinary tract infections, use of feminine hygiene products, Kegel exercises):
none
Male Genital System (penis or testicular pain, sores or lesions, penile discharge, lumps, hernia):
NA
Health Promotion (performs testicular self-exam):
NA
Female Genital System (menstrual history, age of first menses, last menstrual cycle, frequency of cycles, premenstrual pain, vaginal itching, discharge, premenopausal symptoms, age at menopause, postmenopausal bleeding):
- Received first menses at the age of 13
- On menstrual flow 28 days
- Severe abdominal pains
Health Promotion (last gynecological checkup, pap-smear and results, use of feminine hygiene products):
- Yearly check up
- Sanitary towels
Sexual Health (presently involved in relationship involving intercourse or other sexual activity, aspects of sex satisfactory, use of contraceptive, is relationship monogamous, history of STD):
NA
Health Promotion (safe-sex practices):
ABSTAINANCENursing Diagnoses:
Based on this health history and health screening, identify three nursing diagnoses that would be applicable for this client as well as your rationale for your selection of each nursing diagnosis. Include:
One "actual" nursing diagnosis with rationale for choice of this diagnosis.
Actual nursing diagnosis decribes a health problem that is current (Roseman, 2014). In this case it is sleep depreviation. The patient find s it hard to sleep because of the severe pains she experiences during her monthly period.
One wellness nursing diagnosis with rationale for choice of this diagnosis.
This type of diagnosis deals mostly with the patient's readiness to become better (Stolte,1997). Here it is the patient's readiness to play sports so as to reduce the abdominal pains.
One "risk for" nursing diagnosis based on the health screening with rationale for choice of this diagnosis.
Risk diagnosis describes the possible outcome of a certain issue. Here there is the risk for endometriosis as evidenced by severe abdominal pain every other time the patient is on her menses and abnormal growth of uterine lining tissues (ribeiro, 2017).
Rerences
ribeiro, m. (2017, april 24). 6 Possible Causes of Endometriosis. Retrieved from 6 Possible Causes of Endometriosis: https://endometriosisnews.com/2017/04/24/6-possible-causes-endometriosis/
Roseman. (2014, july 9). What is a three-part nursing diagnosis? Retrieved from What is a three-part nursing diagnosis?: https://acceleratednursing.roseman.edu/blog/three-part-nursing-diagnosis/
Stolte, K. M....
Cite this page
Health History and Screening of an Adolescent or Young Adult Client Paper Example. (2022, Sep 20). Retrieved from https://proessays.net/essays/health-history-and-screening-of-an-adolescent-or-young-adult-client-paper-example
If you are the original author of this essay and no longer wish to have it published on the ProEssays website, please click below to request its removal:
- Health Informatics in Improving the Quality of Life Among Patients
- Nursing Paper Sample: Nursing Care Models
- African American women and HIV Prevention Essay
- Atypical Hemolytic-Uremic Syndrome Essay
- Essay Example on Optimism & Positive Affect in Diabetes: Improving Wellbeing & Outcomes
- Essay Example on Nurse Educator Role: An Exciting Transition to Inspire and Nurture
- Essay Sample on Sustaining Patient-Centered Medical Homes: Strategies, Innovations, and Policy Impacts